Joan Rivers was my client around the time of her late husband Edgar’s death. She was referred to me by her ear nose and throat physician Dr. Edward Kantor in Beverly Hills to help her learn to not abuse her vocal cords and to help her use her speaking voice more effectively. So it came as no surprise when I learned today that she went in for an endoscopic procedure at Yorktown Endoscopy Center in NYC so that her doctors could get a closer look at the function of her vocal muscles.
We all remember Joan as having a machine gun like gutteral sounding hoarse voice as we not only heard her verbal jabs during her comedy routines, but her vocal jabs to her laryngeal muscles and vocal cords. When a person sounds hoarse and often lose their voice, it is not uncommon to have a laryngeal endoscopic procedure done so that the physician can visualize the vocal cords to check for how they function or whether there is paralysis, vocal nodules, or vocal ulcers.
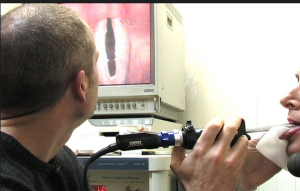
The procedure using a transnasal flexible laryngoscope or laryngeal oral scope is used for this office-based diagnostic procedure which is extremely well tolerated and performed on patients of all ages from newborns to someone who was 81 like Joan Rivers.
Before the endoscope is inserted topical anesthetic is placed in the nasal cavity to avoid stinging and burning during the procedure.Then they sit in an upright position and the scope is passed along the floor of the nose into the back of the throat to a level just above the vocal cords.It is essentially a painfree simple procedure.
Next the patient is asked to breath deeply and say the “ah: sound which allows the physician to directly observe the structure and dynamic motion of the vocal cords which they can view on a video screen .There are no side effects of the procedure and the anesthesia spray usually wears off in about an hour.
So if Joan was undergoing this simple non invasive non life threatening procedure, what happened? Why was her airway cut off? Did someone do the procedure improperly? Was a technician doing the procedure or was it a licensed physician? Was this a case of malpractice? I have to ask these questions because it seems odd to me that her airway would be closed off.
Also lets say her airway was closed off, why did a clinic of this kind or any kind not have life saving equipment to open her airway? If she had a heart attack, why was there no immediate cardiac life saving devices on the premises? Why was she deprived of oxygen for any length of time? Why wasn’t she given oxygen immediately? This bothers me. Why were there not life saving emergency devices available and if they were why weren’t they implemented asap?
I am so disturbed by this for several reasons. First, I knew Joan personally along with her daughter Melissa and I know the horrible toll it will take on Melissa and her son, not to mention the toll it will take on Joan, if she survives.
Secondly I had personal experience with something like this happening in my own family. My dearest brother Manny was intubated improperly by a doctor who was only a doctor for 7 months. As a result my brother became a vegetable and died. I can never get over this and carry this severe emotional pain with me my throughout my life. So I cry for Joan and for Melissa and for her son Cooper as I know exactly how they feel to know that someone they loved had to die or become incapacitated in such a horrific manner.
I have no doubt that with the resources available to Melissa there will be a thorough investigation as to what actually happened and who may be possibly responsible.
It is so devastating that Joan was looking and feeling so good as it was reported hours earlier. Now her life is changed forever- and not for the better .
Joan is now in a medically induced coma and depending on how long she was deprived of oxygen to her brain, she will most likely never be able to do what she did before. For some people that may be viewed as a relief because they found her humor politically incorrect and mean spirited. For others who enjoyed her humor and her views it is a great loss.
Joan’s politics, point of view, and humor aside, no one should be going into a non invasive relatively simple procedure and end up potentially brain damaged in in a medically induced coma where they may never be able to speak or live.


As a medical doctor, I strongly agree that there are many serious and deeply concerning questions regarding what happened in this case. From a medical standpoint, the facts have not yet been made public, however, the explanations offered by the various media sources do not make sense to me from a medical standpoint. All we devoted fans can do is pray that Ms. Rivers has not suffered significant brain damage and that she makes a full recovery. She is a brilliant, talented woman who deserved the very best medical care available.
Dan Laird, MD
LikeLike
Thank you so much for your comment and insight Dr. Laird. It is very much appreciated.
LikeLike
If this Dr. is not certified or things were done wrong, it just surprised me, this is not the Michael Jackson case where MJ knew only few Doctors would give him propafol (sp), so a person like Joan Rivers who has they money could get to a top specialist and she picks this doctor.
LikeLike
Dear Dr. Lillian Glass,
Thank you so much for your comment on this matter. I, too was very troubled by what happened during this routine procedure and I totally agree with you.
I pray Ms. Rivers recovers and there will be a thorough investigation.
Take care now and May God Bless.
LikeLike
Dear Doctor Glass,
I too have been troubled as to why an outpatient endoscopy would have caused such disasterous results. Thank you for your insight into the procedure itself. From watching her on E! this week she was at the top of her game, sassy and very healthy appearing. I admire her comedy career and thoroughly enjoy her QVC design creations. I am sure, Dr. Glass, it was a gift to know her personally.
Sincerely, Dorothy J.
LikeLike
The problem is it wasn’t endoscopy. It was laryngoscopy done in an endoscopy clinic.
LikeLike
You hit it on the head! This is an E.N.T. Procedure not done by a gastroenterologist and not under sedation with an unprotected airway but should have been under general anesthesia with an endotracheal tube to secure her airway by either an anesthesiologist or a Certified Registered Nurse Anesthetist.
LikeLike
Dr G.,
I salute for you outing that thug. I always would use my name to comment, when you click on the avi’s (through Gravatar on a wordpress blog) it would show the profile. I never had anything to hide, I would post my my first and last name on my profile.
To make this long story short, I commented on a blog similar to yours. It was ran by a PROFESSIONAL like yourself. The professional would speak on subjects similar to yours.
With all blogs, this professional had trolls like you have. This professional would invite them to debate as long as it was done with out name calling. I know, she ran a right ship. [sarcasm]
I would stick up for the Professional, one time I got an email from the professional telling me to ignore because it the same person was posting under multiple names and ended up blocking the troll.
I started receiving; hang up calls, disturbing letters in the mail and a few other things happened which I will not get into.
My husband does not play. He went to the authorities. It turned out this troll looked up my name and found where I lived and would taunt and harass me. It was frightening. I knew instantly who it was because she named the professional in one of her cat urine soaked letters. I don’t know
why the Post Office even allowed it to be sent.
It turned out it this lady was a middle aged hoarder with mental problems. While I feel for her psychological problems, it was still no excuse.
I no longer ever comment with my name because of TOXIC people like this one. I can sit and laugh about it now, I guess it’s nervous humor. I will not allow these trolls to define me or stop me commenting – do not ever let these TOXIC trolls from doing what you do either.
I say to you Dr. Glass: GOOD for you! Do not let trolls take over your blog. Please know while these TOXIC trolls spend their lives harassing people like you and you feel like giving up on the blog, know people like myself RESPECT and APPRECIATE you.
That troll is a coward.
Dr. Glass is NOT diagnosing. Dr. Glass is speaking from experience and COMMON SENSE. No one forces you to read this blog.
LikeLike
Thank you so much for your share and your post.
LikeLike
Courage is the word for Joan. She is a smart, funny, clever woman who made her life work against all odds. One more time Joan.
LikeLike
Yes, one more time Ms. Rivers! I wanna hear you joking about this craptastic event the next time you’re on stage here in Vegas! Please let it be! Danial Laird
LikeLike
Here’s a post I found from an otolaryngologist (ENT surgeon). He thinks Ms. Rivers was actually having an EGD, possibly to evaluate vocal cord injury from acid reflux? Perhaps there was a sedation complication?
http://fauquierent.blogspot.com/2014/08/joan-rivers-suffers-respiratory-arrest.html
LikeLike
I am an anesthesiologist and that was my first, second, and third impression as well. This procedure described above is a laryngoscopy, not an endoscopy, and you look at what Yorkville Endoscopy does and the doctors affiliated with it and it’s unequivocally GI endoscopy and every last doctor listed on their website is a gastroenterologist.
Parenthetically, I had a nasal laryngoscopy done on me by an ENT surgeon just as a curb side in the operating room when I was hoarse after a severe cold. He used no topical anesthesia and it was no big deal. Afterwards, he advised vocal rest and (significantly) that I start taking pepcid round-the-clock as stomach acid suppresion.
LikeLike
Dr. Cohen, do you happen to know who generally does sedation/anesthesia for EGDs on the Upper East Side? Is it physician anesthesiologists, CRNAs, or the circulating nurse under direction of the GI doc? Can non- anesthesiologists administer propofol in New York endoscopy clinics? Danial Laird
LikeLike
I’m afraid I do not know. I’m practicing in south texas and had precisely the same questions. Anesthesia colleagues I discussed this with (and some plain RNs) were of the opinion nobody trained in anesthesia could possibly have been involved in this. I’m inclined to agree. The center states they can not define when Ms Rivers was no longer oxygenated, which to me means she was not monitored during the episode (at least with pulse oximetry). And that’s a standard. I do not know anybody in the specialty who would practice like that.
I did do a search for nurse administered propofol to try and see if the state has a position on that. The GI docs have been pushing for it for some time, as I’m sure you’re aware. I did unearth a position paper from the NY nursing board stating nurses with appropriate training could use propofol on ventilated patients, but came away with the distinct impression regular RN propofol administration in unventilated patients was verboten as it is here in TX. However, as I’m sure you’re aware, you can do precisely the same thing, perhaps less reversibly with versed/fentanyl particularly in an 81 year old where I’ve personally seen octogenarians go “under” with tiny versed doses and stay that way a long time. Granted, you do have the crutches of narcan/romazicon but the romazicon won’t outlast the versed and narcan has some substantial drawbacks/risks particularly if administered as stupidly as the original opiate was.
Long winded answer for which I apologize.
LikeLike
Thanks Dr. Cohen! If the facts of the case are made public it will be interesting to hear what actually happened and who was involved. Danial Laird
LikeLike
I hope there’s a law suit that makes it to court. That will make me very unpopular with my colleagues, but I think that may be the only way we’ll find out in public what happened here. I have this vision in my mind of some regular RN pushing propofol at the direction of the endoscopist. The “system” is pushing in that direction, and the facts I’ve heard are lining up to support it. But it would be better to know for certain.
LikeLike
Dr. Cohen thank you so much for your integrity and for saying this as I completely agree that there needs to be a lawsuit. In fact the latest is that the family is indeed considering a lawsuit for the botched procedure as you see in this link
http://www.nydailynews.com/entertainment/gossip/joan-rivers-brought-medically-induced-coma-source-article-1.1923394
LikeLike
New York City Endoscopy Centers are well known to present significant dangers to patients. I ask myself why would a gastroenterologist associated with the Yorkville Endoscopy Center be doing a procedure on Ms. Rivers. Playing with the vocal cords can lead to laryngospasm and negative pressure pulmonary edema. Endoscopy centers do not carry the drug required to break laryngospasm, succinylcholine. They do not have the drug in the possession because having it also requires that you possess the drugs required to treat Malignant Hyperthermia and the machinery to diagnose the disorder as well. Endoscopy centers do not carry these drugs because of the expense of the ones to treat and diagnose Malignant Hyperthermia.
There is another Endoscopy Center in Manhattan that has been under both Federal and State investigation for almost three years related to a False Claims Act filing in a Manhattan court. That case related to the owners of the Endoscopy Center dictating to anesthesiologists that they should lower ASA risk assignments so as to increase business by performing procedures on patients who are excluded by NY State law from being treated at the specific facility. There was another prominent patient, Mr. Elie Weisel, injured who was also sent to Mt. Sinai Hospital. Mr. Weisel was downgraded from ASA 4 to ASA 3 at the insistence of the Chief Medical Oficer who also preformed the endoscopic procedure which resulted in Mr. Weisel going to Mt. Sinai Hospital in cardiac distress.
LikeLike
WOW! Thank you for the eye opener and sharing this valuable information.
LikeLike
New York City Endoscopy Centers are well known to present significant dangers to patients. I ask myself why would a gastroenterologist associated with the Yorkville Endoscopy Center be doing a procedure on Ms. Rivers. Playing with the vocal cords can lead to laryngospasm and negative pressure pulmonary edema.
Did you see on ET… I can’t remember the Dr’s name, but the way he described was, someone like Joan who has had many procedures with the nose area.. The Dr said, the vocal chord area is round and large enough for a the endoscope to go in, when you insert the endoscope usually it has area to move around, he then said, with someone like Joan who gets allot of work done the area can shrink over time.. that could have happened when the endoscope was inserted when they entered the area the and endoscope it could have immediatly stopped her breathing. You make a very valid point
New York City Endoscopy Centers are well known to present significant dangers to patients. I ask myself why would a gastroenterologist associated with the Yorkville Endoscopy Center be doing a procedure on Ms. Rivers. Playing with the vocal cords can lead to laryngospasm and negative pressure pulmonary edema.
LikeLike
I have considered succinylcholine an emergency drug on the same level as epinephrine and atropine specifically because of the scenario you cite since my residency. If I had been working in a situation where an administrator dictated regrading of a patient like that, I would feel morally obligated to dismiss myself from the case and the center on the spot. That’s reprehensible. But if they didn’t carry succinylcholine, I wouldn’t do an anesthetic there to begin with.
It’s true there are other ways to break a laryngospasm (IV Xylocaine, more propofol, positive pressure ventilation), but personally I use sux early rather than late. It works immediately and well in almost all cases.
That’s just me however.
LikeLike
I would like to make clear that NY State surgicenters are prohibited from treating patients classified as ASA4 or greater. It would be interesting to know more about what occurred at the Yorkville Center. The center is physician owned exclusively by gastroenterologists. There fore, I would think that Ms. River’s procedure was undertaken by a gastroenterologist which then opens the question of his institutional credentialing and training related to an examination of the vocal cords. Laryngospasm when encountered is a serious matter which requires some level of advanced preparation. Endoscopy centers in Manhattan are very heavily influenced by a consulting firm called Friedlander and Associates. Dr. Charles N. Friedlander is the CMO at the center associated with Mr. Weisel’s care. As I noted his center is under State and Federal Investigation related to a federal court filing.
The endoscopy centers are not equipped for the delivery of anesthesia like a hospital. There is no succinylcholine, There is one pressure controlled ventilator without PEEP capability. There is no means to place a percutaneous cricoid catheter and to jet ventilate a patient. In reality, there is no person with the knowledge or equipment to perform a cricothyrotomy to relieve a laryngospasm. New York State does not do a good job at monitoring Endoscopy Centers. Quad A, Triple A and JACHO do not do a good job as they are focused on the paper work and policies leaving the operation of the facility to the physician owners.
Propofol made these Endoscopy Centers possible. They hire inexperienced CRNAs and new anesthesiology grads along with those who want to work in an environment with no call or direct responsibility. The Anesthesiologists are an salary and not partners in the practice. Ms. River’s family likely has a good claim against the caregivers at Yorkville Endoscopy ans well as the Center and the agency that provided accreditation..
LikeLike
succinylcholine. disappears from the system fast, can it be even detected? I think unless you look for it that it would be.
LikeLike
Of course we are all praying Ms. Rivers makes a full and complete recovery. At this point, there are just too many unknowns to draw conclusions about what happened. Whether any doctor or nurse performed below the standard of care cannot be determined by snippets of information and misinformation reported by the press. I agree, however, that the outcome is unusual and there are many concerning questions to be asked by Ms. Rivers and her family. I think this blog is useful as a forum for the exchange of ideas; all her fans want to know what happened. Danial Laird
LikeLike
Hi..I was wondering to whomever can answer. I had a camera in my nose but not down to vocal cords. I have to do it again. My question is. ..is there risks w getting a camera put down there…thru nose to vocals? And how do you spasm and get an airway blockage by doing it? I’m sorry but I forgot what it’s called. .the spasm is misdiagnosed for asthma. So are you pretty “screwed” if your vocal cords close on their own? I’ve been given exercises to do for it. Just random questions. I hope Joan gets well. Sad to see anyone go thru this. Thanks
LikeLike
“no one should be going into a non invasive relatively simple procedure and end up potentially brain damaged in in a medically induced coma where they may never be able to speak or live”
In her case I guess that wouldn’t be much different from usual, heh. You might say her clearly toxic personality got the better of her.
LikeLike
No, I wouldn’t say that Pat Maybeck. Joan Rivers graduated college with honors and is known to have an exceptionally high IQ. She also has a sense of humor. Regrettably, it’s obvious you don’t. Ms. Rivers has been extraordinarily generous with her success. Her work with God’s Love We Deliver is well known nationally. The fact that she took care of patients with AIDS, when few other people would in the 1980s, speaks of her character. In my mind, she’s basically a saint. You are no Joan Rivers. Danial Laird
LikeLike
You are barking up the wrong tree Danial. Joan Rivers having a toxic personality later in life has nothing to do with her graduating from college with honors and having a high IQ. Furthermore, it has nothing to do with her previous acts of charity. The proof of her toxicity is in the media, both printed and in front of the camera. There are certain things which cease from being funny regardless of how they are said and regardless of the context.
A person having a toxic personality and that toxicity getting the better of them has to do with what is in an individual’s heart, not what they want people to believe about them by what they have done in the past.
To call Joan Rivers a Saint is insulting to anyone who truly understands what qualifies a person to be a saint and to the individuals who actually were. Mother Theresa was not even qualified to be a saint, yet she dedicated her life to helping people, died penniless and never made any statements which could ever be remotely construed as racist, insensitive and just plain cruel.
LikeLike
First, I’m not going to reply to any attacks again myself, the md’s here or Joan Rivers though I do need to reply to Peter.
This is medical info board. It was posted that the md’s here are sharing the benefit of their expertise so that her fans have some info to make it a little easier. They did – on both counts though it’s still not easy.
That said, I think you need to ask yourself what kind of person picks a fight with md’s trying to help against an 81-yr woman who is lying on life support and completely unable to defend herself?
It may just be, Peter, the same kind of person who can’t listen to what she said – which people are saying all over the place in their own words – often far worse than anything she said ABOUT THOSE WHO ALREADY SIDED _AGAINST DEMOCRACY FOR THEIR OWN PEOPLE_ (and were killed anyway).
As long as you have a volume control, no one is toxic to you unless you let them but THAT is not something you can do for yourself but, for all her fans….tune out if you don’t like it but don’t blame what you won’t do on her and especially not now!
———————————————————————————-
I hope you kind medical people will continue to share your medical opinions for those of us who don’t understand how this happened….and thanks!
LikeLike
I also wanted to address the TOXIC hatred I have read in comments throughout the internet about Joan Rivers. Whether you liked her humor or not, she is still a human being and to say things like “she can’t die soon enough” as hasssan2 stated is disgusting and shows a complete lack of humanity and character.
Exactly! There are tons of ppl who I don’t like that are public figures, but my goodness! I don’t want them dead or anything bad to happen to them.
Dr. Glass,
You are too funny.. I am so proud of you.. Good for you! I would like to give you a helpful tool for this troll of yours but do not want to say it on an open forum – I have a feeling this idiot will continue this, they don’t stop. Trust me, I have them on my site.
Anyhow, my email addy is on my comment. If you want, send me an email so I can show you something. No, i am not an obsessed fan, LOL!. I’ve been reading your blog for years and always watched you on TV when you are called as an expert.
LikeLike
Dr. Glass,
One last comment, a friend of mine who works in the medical community is reading your blog and set her phone to my WIFI, you may get another comment from my IP.
LikeLike
Here’s some good news!
http://artsbeat.blogs.nytimes.com/2014/09/03/joan-rivers-moved-out-of-intensive-care/?_php=true&_type=blogs&_r=0
Danial Laird
LikeLike
Supposedly moved to a private room but “still on life support” whatever that means… probably intubation and mechanical ventilation. At some point, if she survives, I imagine she’ll need to go for a PEG/Trach if “life support” is to be maintained. After a week or so patients mouths get pretty beaten up.
LikeLike
The most recent update from the Rivers Family says she’s been moved from the ICU to a private room. There was no mention of life support. Of course I have no personal knowledge of the situation, however, I believe this means she is no longer intubated and being ventilated on a machine.
In my mind, it means one of two things. One possibility is that she’s made substantial progress and doing much better. The other is that the injuries were so catastrophic that life-support has been withdrawn and only comfort measures are being offered. I pray the situation is the former. Danial Laird
LikeLike
“Melissa also confirmed that “at this time [her mother] remains on life support.”
http://dailydigestnews.com/2014/09/report-joan-rivers-moved-to-private-room-at-hospital/
It could simply mean they can’t do anything more for her in the ICU.
If she’s badly injured, I hope she dies. There are things worse than dying.
LikeLike
Dr. Cohen, the article you’re referencing combines the updates of Sept. 2nd and 3rd. Melissa did say both of those things but on different days. The text of what was released each day is at http://www.joanrivers.com. In the usual vernacular, in my experience, “life support” means the trachea is intubated and the patient is mechanically ventilated. I may be wrong, but “out of the ICU” to me means no longer intubated or ventilated. Now, that may be because she no longer needs to be ventilated or sadly, because there is no hope and she’s only being kept comfortable prior to death. This is all merely speculation. This is a world class celebrity with unlimited resources in one of the finest hospitals in the world. Perhaps a ventilator was set up in a private room; it’s possible although in 20 years of practice I’ve not seen that done. I’ve anesthetized a number of well known athletes and celebrities over the years. I am a strong believer that the chance of something going wrong dramatically increases when health care providers get off their game and change their usual routine based on the celebrity status of a patient. Hum drum, ho hum, boring as hell; that’s the way a celebrity case should go.
LikeLike
How about this one?
http://www.nydailynews.com/entertainment/gossip/joan-rivers-private-hospital-room-professionally-decorated-friend-article-1.1927433
I absolutely agree on the issue of VIPs and clinical objectivity. I was once called to care for the dean of the medical school while on-call. There was considerable nervousness as we (doing the case with a resident) received no fewer than 5 phone calls from our department chairman between holding area and operating room. You never ever compromise or change your standards saying, “I’ll just use a smaller IV or endo tube this once.”. Never ever ever. Treat everyone exactly the same neither better nor worse. In our attempt to treat better, we may well treat worse.
Our dean obstructed his airway after extubation and I used a nasal trumpet on him too. He turned out fine. I don’t care if surgeons/patients/g-d almighty hate the things. I think the person who created them was a genius.
LikeLike
I’m very conservative but I won’t even have an EGD or colonoscopy without a board-certified physician anesthesiologist administering the sedation, and that doctor has to be hand-picked by me. Next time I need a procedure I’ll call you Dr. Cohen! If there is any good that can come out of this sick tragedy, perhaps it will be that the public’s awareness of the seriousness of “minor” medical procedures requiring sedation or anesthesia. Danial Laird
LikeLike
Today, I was doing an anesthetic for an EGD, the patient obstructed her airway. the usual chin lift didn’t help and her saturation crashed. I started placing a nasal trumpet and the GI doc protested, “I hate those things. The patients complain. Don’t do it. I won’t be long…”. My answer: “thank god the patients live to complain, they are my favorites short of an LMA or endotracheal tube. And if Joan Rivers had one, she’d still be doing the “fashion police”. He shut up, I placed the trumpet. The patient got better.
LikeLike
Good for you Dr. Cohen! A friend of mine who is an anesthesiologist tells the story of having to physically push a gastroenterologist away from the airway when the patient was desaturating. Assuming there is an anesthesiologist present, it is his or her responsibility to ensure the patient has an airway regardless of what the endoscopist or surgeon does. I believe that sometimes proceduralists get so concentrated on what they’re doing they forget to look at the overall picture and take into consideration the overall well-being of the patient. Of course we have no idea what happened in this case. The facts are not yet publicly known.
Danial Laird
LikeLike
Some of the media are reporting that the endoscopy clinic where Joan Rivers had her procedure is being investigated. I suppose this is a good thing to the extent the investigation will be objective and uncover the truth. The general consensus among media pundits seems to be that Ms. Rivers has suffered catastrophic brain injury and that she’s receiving “comfort care” AKA “hospice care.” Whether medical error led to this sick tragedy is not known; the facts have not been made public by those who are in a position to know. The circumstances surrounding her injury are extremely concerning. For the sake of her family, I hope there was no medical error. Perhaps it’s easier to grieve when there’s nobody to blame? I don’t know. Danial Laird
http://www.foxnews.com/entertainment/2014/09/04/joan-rivers-clinic-investigated-ny-dept-health/
LikeLike
Speaking generally, the sort of mistake that leads to a truly catastrophic outcome, as this seems to be, isn’t the result of a single blunder or even a single individual. It tends to be “the system” in some shape or fashion, even though an individual may have contributed. That’s the basis for modern QA and use of sentinel events (this qualifies). That’s where the NY Health Dept should be looking. Given that it’s an organ of government, I’m not optimistic.
LikeLike
I agree with your analysis Dr. Glass. As for folks like “Peter,” I don’t even think they’re worth a response. If he were lying on your couch and you were shrinking his head, he’d probably eventually admit, “My mama didn’t teach me no better.” As Maya Angelou said, “When you know better, you do better.”
Everyone places his or her line at a different point, depending on probably how s/he sees the world. For me, Ms. Rivers has never crossed the line. Her response to critics has been, “For God’s sake, it’s a joke, OK?” If someone is offended by the humorous assertion that the President is gay, it says more about the joke listener than the joke teller. Rivers would say, So what if the President is gay, who cares?
Joan Rivers is an amazing woman on so many levels. I’m no fashion aficionado by any stretch of imagination so I don’t appreciate her expertise in that area, but I think she taught the world that your best years can be the 50s to the 80s. She’s also repeatedly persevered in the face of adversity. She’s always been ahead of her time and I don’t think many people appreciate how extremely intelligent she is. I saw her perform not long ago and was absolutely amazed at her quick wit, incredible memory, and generosity to the audience. She’s a sophisticated entrepreneur and has been extremely generous with her success. She’s someone worthy of admiration.
LikeLike
I love jr but thank g-d she died. It could have been worse.
LikeLike
It is very true as she would not wanted to have lived in the condition she would have ended up being in.
I also thank you so much for all of your wonderful comments and insight.
LikeLike
May she rest in peace.
LikeLike
This is a video of an amazing interchange between Melissa and Joan about dying right before Joan went in for one of her plastic surgeries in Beverly Hills. We seeherr raw open and honest allowing herself to be filmed without a stitch of makeup. What is saddest is that she didn’t expect to die under this minor procedure in a NY endoscopy clinic.
LikeLike
This is very moving. We all know that reality shows are scripted, but the special bond between Joan and Melissa really comes across here, and I believe they are sharing their true feelings.
What a sad irony that she would survive so many unnecessary surgeries, only to succumb to a routine, low-risk procedure. Hopefully, for the family’s sake, they will get to the bottom of what really happened.
LikeLike
This Whole Case sounds so Suspicious…
Seems like she was chocked/pressure maybe put on her Carotid artery during the procedure?!
This could cause a Cardiac Arrest…
The 911 call & Code Blue seemed to be a bit slow/delayed…
Why wasn’t CPR Initiated at the MD’s Office?
I work in Health Care & what ever Happened seems off.
They should have checked her vital signs before the procedure
I was Hoping she would pull through…
RIP Joan
LikeLike
Chocked? Haha, are you trying to say they were trying to kill her? Why in this world would you want to put pressure on her carotid for an endoscopy? You sound like a very ignorant “health care” worker.
I’m pretty sure they started CPR in there or else she would not have even made it to the hospital and ICU.
How do u know they didn’t take her vital signs? Where you there?
LikeLike
You weren’t there either,so you don’t know what happened and can;’t be sure they started CPR. She made it to the hospital all right- in a coma.
LikeLike
Dr Glass,
I am devastated by the loss of Joan Rivers. Joan’s vitality, and youthful spirit was an inspiration to us seniors. Her comedic gifts brought laughter and endeared her to our hearts. It is hard to believe or take that Joan is gone. Shame on the Yorkville Endoscopy clinic if they caused her tragic loss and as such, need to be held accountable. We love you Joan and will hold you in our hearts forever.
Elizabeth Kelly – September 4, 2014
LikeLike
Very glad to have found this site. What a horrible, completely senseless loss today. I am a JR fan, have been since I was a kid.
I am also a BC Emergency Medicine doc. From the start I wondered about the “cardiac arrest” story because it was intermittently swapped out with the “stopped breathing” version. I thought it was possible that stopped breathing, desaturated (blood oxygen plummeted) and, as a result, gone into cardiac arrest.
What I couldn’t understand is 1) why no one picked up on the decreasing oxygen levels – I assumed, obviously incorrectly, that a patient undergoing a procedure under conscious sedation was on continuous monitoring and that an R.N. or M.D. had the responsibility of recording changes & taking notes as the procedure was performed. 2) I didn’t ‘get’ how Joan Rivers’ otolaryngologist didn’t immediately intubate or have an anesthesiologist standing by who could.
I started to wonder if advanced airway equipment and RSI (rapid sequence intubation) medicines were even available AT BEDSIDE or not. In the ER, we are held to very clear rules for any procedure involving conscious sedation. If I am ready to do a procedure – from reducing a dislocated joint to inserting a chest tube, I can’t and wouldn’t proceed without the patient being monitored, an RN whose only duty is watching the patient & the monitors, a crash cart in the room, and my own ability to intubate the patient.
If I believe the airway could be complicated (based on the patient’s anatomy or history), I wait for an anesthesiologist who is able to stand by or have a surgeon take the patient to the OR, where there are many anesthesiologists available and the procedure can be done under general anesthesia if needs be.
The most dangerous thing in medicine is a doctor who does not know his/her limitations AND doesn’t understand the risks that go along with the procedure that’s being done.
You can do a particular procedure 10 times without incident. That doesn’t make the 11th one any less risky for occurrences out of your control. We don’t stop using seat belts because our last 100 car trips didn’t involve a crash.
How dreadful that ANYONE had to die because of ignorance. It is finally clear to me that Joan stopped breathing; It wasn’t noticed until maybe a minute later when her heart stopped; They likely used an AED to get her heart going again; She likely had no definitive airway until she got to Cedar Sinai & by then she was brain dead.
Joan, my husband and I will miss you. We watch you every week on FP. I send love to you and your family.
Go start telling them off in heaven…Tell Robin and Michael and Whitney and Diana to get the hell back down here. I’ll wait for YOU to show up and tell us this was a really tasteless joke…..”too soon?”
sigh…
LikeLike
Those “clear rules” you talk about are also followed by outpatient surgical and endoscopy centers. Your assumptions could be correct as far as the cause of death but you are an ED physician and not ENT or anesthesia, you don’t know what they had in their hands so stop assuming they committed malpractice. You don’t know!!
LikeLike
Questions about malpractice definitely need to be asked because someone who is vital and vibrant needs to come out of the facility alive and functioning not in a coma.
LikeLike
I know a few things about surgical care and anesthesia. I also know about the structures of practice in New York State. Yorkville Endoscopy is a GI center. It is doubtful that their NYS facility license includes procedures on the vocal cords. GI doctors do not do such procedures and are not trained to do such procedures. I would think that Ms. Rivers signed a consent for surgery, but then I would question whether she could have had been given informed consent for a procedure planned at a facility not licensed to do such procedures. Also Ms. Rivers would have signed a document acknowledging that she was aware of the procedurist’s financial interest in the facility. Taking the financial interest and the performace of a procedure beyond the facility’s NYS license should lead to the closure of the facility in a normal universe, but not in NYS. I am aware of another NYC GI facility that is being investigated since 2012 without resolution.
LikeLike
Emergency doctors work closely with every specialty in he hospital. Do you think that in 9 yrs of medical school, internship and residency I never worked with ENT or anesthesia? Both required rotations in Emergency Medicine residency? Do you think that in 16 yrs of practice I don’t see and work with these colleagues? You are clueless as to how a hospital functions.
Whatever they did or did not have in their hands, Joan Rivers entered in good health and left their facility brain dead. Not being prepared for a lethal complication is malpractice.
I appreciate the comments of Dr. Glass, below.
LikeLike
STP… you’ve probably figured this out but the reply after yours was to David, not you. I appreciate your informative post.
LikeLike
Reblogged this on bonniesblogsite's Blog and commented:
This is interesting insight from a physician who knew Joan Rivers.
LikeLike
Respiratory arrest likely occured first. The staff present was not able to get a continuous oxygen supply to her lungs within a couple minutes of the witnessed event. The consequence is cardiac arrest shortly, within seconds to minutes( it can vary)The breathing must be restored within a couple minutes to prevent a cardiac event eg ( heart stops) because brain cells start dying immediately and quickly. It appears the respiratory part wasnt corrected which led to the heart stopping. It takes alot of experience to correct a respiratory and cardiac event in the ER Surgery or med surg ,but for it to occur in a doctors office is a disaster waiting. One needs not only Certified staff but needs specific training on the job with these type events to be reasonably competent. Its highly unlikely that the staff present had any actual hands on experience with an event like this. Correcting her problem required very specific experience with this type emergency. Experience of this sort is usually attained by many/not all EMT or paramedics,or RNs that have specific experience in ER or ICU and OR. Anesthesiolgists or Respiratory practitioners are the most experienced in this area ,but respiratory is usually closer to respond and there are more of them available than anesthesiologists so they are called first.
Any event of this serious nature requires quick and effective choices /decisions and its just not going to be available if youre in an office with 2 or 3 staff that passed cpr class.
LikeLike
That is exactly what I was said Timbuc. FYI, EMT’s do not do intubations.
Paramedics are almost always adept at the procedure. In my experience, Flight nurses are second to none….other than the anesthesiologist on steady ground, with advanced equipment at the ready. An anesthesiologist, an experienced Paramedic (or Flight nurse) should be standing by when any procedure is done on the throat. It is incomprehensible to me that this was not the case.If someone know how to treat laryngospasm & been able to insert even a nasotracheal tube, Joan would probably be talking to us from her bed tonight.
So people understand who does what: Emergency departments staffed by doctors who are residency trained in emergency medicine absolutely have the capability to intubate. They should be able to do so consistently without complications. On the other hand, “ER” doctors trained in primary care (pediatrics, family medicine, internal medicine) and not trained in EM are usually not well prepared for intubations. The non-EM-specialized “ER” docs I have met are not comfortable with the procedure. The exception would be pediatric intensivists in designated children’s hospitals or in pediatric ICU’s. Check the backgrounds of the staff at the ER closest to you. Go to your state medical board’s website and look up the profile of your emergency doctors. Know where you’d prefer to be taken in the event of a serious breathing, neurological or cardiac issue. If you have a preference, ambulances take you to the hospital you request
I always rely on the help of respiratory therapists for assisting while I intubate. If I needed to, I could manage with one nurse or paramedic to administer medications, on a moments notice. If I had to, on my own, I would perform a cricothyroidectomy (have done just one in my career – it saved a life with an intact brain). That procedure was taught on our trauma rotations.
You are right timbuctoo, airway management is not the result of a 1 or 2 day cpr course or any other quick initiation (ATLS or ACLS). For ER docs, it takes 3 years of a certified Emergency Medicine residency, which includes rotations in anesthesia, trauma and, of course the emergency department – at first we observe numerous cases, then we “do” with senior residents, attending doctors and respiratory therapists literally standing against us, guiding us & ready to push us aside & take over until one day, we “get it”. Always under close supervision we practice, practice, practice. By the second or third year comes increasing degree of mastery handling complications that arise and just dealing with a wide variety of sometimes crazy situations. Our cases are not scheduled like those handled by our anesthesiologist colleagues in the OR.
Hope that clears up who intubates and who doesn’t. An elective procedure on the THROAT should be done by an otolaryngologist …omg, left them out!….in a hospital OR with anesthesiologists and RT’s in the room or seconds away.
LikeLike
LRE
Your quote(FYI, EMT’s do not do intubations. )I guess i should have said im in the Republik of Kalifornia. Some of us do. I started out years ago in a rural setting where we did it much more than in the larger cities. And I meant to mention too as you did ,that some ,many or most?? flight nurses and all Flight Respiratory are competent with intubations. The laws here in Kalifornia allow RTs to do intubations in the facility,and for EMTs or paramedics it did a few yeas ago,at least they brought the patient in intubated and one of them did it. Now they use LMA or whatever,it really depends and varies with each state law and each hospital s policy …ok so I think we medical profs agree there should be a better system set up,to minimize the pnt risk.
The MDs should be required to take concious sedation pnt to the hospital..or staff and equip their office to that level risk reduction protecting the patient.
LikeLike
A rotation in anesthesia and ENT does not make you one of them. You may know the basics of their operations but that’s it! Only BASICS! OBGYN doctors also have “rotations” in general surgery and by no means does it make them proficient at it. Most of them are terrible at managing complications and rely on a general surgeon when they mess up. Let them speak for their own profession. ER doctors are great at saving some lives but are also great at missing problems, so don’t come up and talk like you are some sort of ER god. You are just a person and prone to make the same mistakes or judgement errors as other humans.
LikeLike
David thank you for not leaving me out of the circle of fine people you verbally attack. Absent you, I see I am in good company.
LikeLike
Ok,Im an RT and learned emergency,oral or nasal intubations in ER ,OB or on the floor beginning in 1976. In emergencies I do infants ,adults and children if no MD is available. Theyre usually not and ones that dont feel comfortable are fine with someone else doing it .I In my prior posts I tried to keep things shrt,and brief,from a technician point of view & there are many things i just couldnt get into or didnt mention and dont need to or Id be here all day. The general public have no clue what happens in a hospital,how things work etc and there frankly isnt the time to peel the onion of details needed until every non expert is satisfied . In my state(Ca) very few RTs these days intubate ,as it is a difficult risky proceedure to be successful at in an emergency situation.
In closing,as Ive said earlier, ive explained my view from a technicians view and the docs have given theirs .that should be enough.
LikeLike
This is troubling and should never have happened. Joan Rivers gave us laughter so that we could survive sad days she made a difference in the only way she knew how to and that was through laughter. I am saddened yet again . she is gone too soon RIP @Joan rivers
LikeLike
Are u a doctor or a lawyer? Bc you sound like a very biased doctor or a greedy lawyer. Your assumptions are mostly incorrect and very laughable for a medical professional. I’m pretty sure the facility she was being treated in had appropriate life saving equipment as she would probably go for no less. I understand you do some procedures under local only but thousands of people in the US opt for sedation on many procedures even when it is not needed. Finally, sorry about your brother, but what does seven months in practice have do do with his death? It could have been a 7 year practicing doctor. You are wrong and need to reframe your thinking.
LikeLike
First of all David if you would have read the first sentences of this blog you would know that I am neither a physician nor an attorney but a voice and communication expert who treated Joan for her raspy voice years ago.
Secondly you cannot be sure of anything regarding whether her life saving facility had appropriate life saving devices unless you worked there and were personally responsible for the upkeep of these life saving devices.
Thirdly as far as my brother is concerned and your question about what being a doctor for seven months has to do with his death, the doctor was inexperienced and never did the intubation procedure before and he did it improperly and suffered the consequences for in essence killing my brother. And you clearly missed the point again in the article because you neglected to read the part concerning my brother.The only reason my brother was mentioned in the article was to express how deeply I felt the emotions that Melissa must be going through as I have been in the position of watching someone I love die due a medical procedure.
And finally you have right no to tell anyone they are wrong and need to reframe their thinking as those words could easily be said to you. You need to reframe your thinking and take your Toxic contentiousness elsewhere.
LikeLike
IMHO, the questions that need to asked in this case are the following:
1). Was there a physician anesthesiologist or nurse anesthetist present for this procedure?
2). If there was no MD/DO anesthesiologist, or a nurse anesthetist present, who administered the sedation/ anesthetic?
3.) Was the intravenous sedative/ hypnotic drug, propofol, given in this case?
4.) If propofol was given, who administered it?
5.) If Ms. Rivers suffered respiratory arrest (very common and expected with propofol), was the airway managed appropriately in a timely fashion?
6.) If no anesthesiologist or anesthetist was present, who billed, or was going to bill, for the sedation portion of the procedure?
7.) Is there any reason an endoscopist would NOT want an anesthesiologist or anesthetist present, providing sedation/ anesthesia and immediately available for resuscitation should the need arise?
8.) If propofol was used in this case, have any of the physicians on staff at the involved facility published studies and position papers arguing that gastroenterologists can administer propofol to endoscopy patients safely, in other words, without the need to have an anesthesiologist or nurse snesthetist present?
Danial Laird, MD, JD
LikeLike
Great questions. Thank you Dr. Laird.
LikeLike
Now ,you know what youre talking about. David hasnt a clue about the real readiness required for risky proceedures and he wouldnt unless he worked hands on in the specific field. Questions of ignorance would be fine,but spouting opinins with no specific experience is idiotic . As evidence by his recent statement: >(Your assumptions are mostly incorrect and very laughable for a medical professional. I’m pretty sure the facility she was being treated in had appropriate life saving equipment as she would probably go for no less. ) That is an idiotic assumption that all Dr offices and,yes even medical centers,doing risky procedures want the public to think,but is oftentimes far from the truth .
Dave has no idea what he’s talking about and just serves to irritate experts in the field with those stupid idiotic opinions he stated.
In any room where any cardiopulmonary intervention may be a consequence ,too many times, errors can be made in the daily check of of emergency items missing or not functioning properly.
Check lists for intervention supplies are critical to avoid complications especially if they can deteriorate quickly resultung in death .
Dave save your opinions for an area you clearly have experience and knowledge.
This is why I rarely get involved with discussions online,because anyone can jump in and comment. if theey limited it to questions that might be fine,but the ignorant opinions,statememnts and the troll like behavior by some is too much to handle.
I guess the only way to really prevent this is when people like dave start in ,we shouldnt take the bait by replying . He survives on verbal conflict and to deprive the tumor,parasite etc of its food supply,will cause it to go away.
LikeLike
I was so saddened to hear of Joan Rivers passing. I recently lost my mother due to a medical error and Joan’s bubbly personality on various shows got me through a terrible time. I am grieving for Joan’s family. Her death seems so senseless. I know “why” will be forever etched in Melissa’s heart and soul. Please know we all feel the loss. I prayed the outcome would be a miracle. Untimely deaths are so difficult to grasp. My condolences, Cris
LikeLike
Chris so sorry for your loss and thank you for your post.
LikeLike
Thank you!
Sent from my iPhone
>
LikeLike
No clear cause of death on the post means “anesthesia clean kill”. Toxicology results are useless a week after the arrest. Did Joan die because of her anesthesiologist or because one wasn’t there?
LikeLike
omg how unprofessional for someone to stoop so low i cannot believe what i am reading from ms glass
LikeLike
Nancy no one is “stooping to any low” as you ridiculously state. There is nothing at all unprofessional about asking questions as to WHY a person went in ALIVE for a minor procedure and came out DEAD! If that happened to anyone in your family you I hope you would be asking the same questions.People should not die from this procedure! So please take your animosity out elsewhere like on those who may possibly have in some way been a factor in her death and not on me or what I said.
LikeLike
Yeah, 81 year old patients with possible risk factors should ALWAYS come out clean when they undergo stressful procedures and procedural sedation. What world do you live in? Go ahead and work in trying to fix the system. Good luck!
LikeLike
How low to stoop to addressing a PhD as “Ms”. I am reasonably sure Lillian Glass would choose “Lillian” or “Dr. Glass” over “Ms” any day of the week. I can’t fathom what Dr. Glass said that you find unprofessional.
LikeLike
Thank you for the information shared by the many experts participating in this discussion. I will share your responses with my radiologic technology students.
It seems toxic personalities and comments abound even in an informative discussion concerning an unexpected death of an extremely intelligent women
who had the capability of making millions of people all over the world laugh. What is wrong with that? Nothing. Make God laugh Joan.
Prof. Virginia Mishkin, R.T.(R)(M)(CT)
LikeLike
Yes, an inconclusive preliminary autopsy finding is not surprising at this point. The relevant toxicology may be from blood samples taken at the time of initial admission to the hospital, and I would think those would have been secured by the ME. Life support was withdrawn because of hypoxic brain damage.
The real question is what caused the cardiac arrest that led to the anoxic brain damage. Pathologists would likely have seen clogged coronary arteries if she’d had an acute myocardial infarction or “heart attack” during the procedure. This probably means the cause of the cardiac arrest was an arrhythmia or Pulseless Electrical Activity (PEA). The paramedics would have recorded the cardiac rhythm they found her in at the time of their arrival to the involved facility. A primary cause of PEA in this type of setting is hypoxia from a respiratory arrest. There are several other causes as well.
It would have been irresponsible for the Medical Examiner to have reported anything other than an inconclusive preliminary cause of death based only on gross examination of the internal organs unless there was some obvious finding such as a punctured lung, breathing tube inserted into the esophagus, or a fresh myocardial infarction. It appears there were no obvious causes of death based on gross examination of the remains.
The more interesting story will come when the ME examines the circumstances surrounding her death and possibly, the toxicology results. Let’s see what the final autopsy results are.
Danial Laird
LikeLike
Hmmm… This sounds a little familiar:
http://www.outpatientsurgery.net/outpatient-surgery-news-and-trends/general-surgical-news-and-reports/what-caused-joan-rivers-to-stop-breathing-during-an-endoscopy–09-05-14?utm_source=news&utm_medium=email&utm_campaign=tji
LikeLike
You’re either a certified body language expert (as I had always believed; I’ve watched you on TV and followed this blog for your opinions on celebrity body language exclusively, and this blog itself is called “drlillianglassbodylanguageblog,”) or you’re an certified medical expert on physician-related vocal medical procedures. Which is it? Also, your posts are often very difficult to read due to poor sentence structure, spelling, and/or grammar.
Catherine
LikeLike
To answer your question Catherine Van Harren I am a body language expert and communication expert who treated Joan Rivers for her vocal problems years ago. Being very familiar with layngoscopy to analyze vocal problems of my patients I posed several questions that needed to be posed. It was a simple procedure where no one was supposed to die. Also having gone through a situation where my dear beloved brother left the hospital a dead man due to improper intubation, I feel extremely qualified to write about the emotional toll this will take on family members.
In continuing to answer your
question about my background and qualifications, I am also a mediator and ligation consultant, expert witness, lecturer, and author. To learn more about my background and to answer further questions about me feel free to look at my wikipedia
LikeLike
I see.nothing about anesthesia staffing in that article. That’s a key question.
LikeLike
Also, your posts are often very difficult to read due to poor sentence structure, spelling, and/or grammar.
Dr Glass writes her own blog, gawd forbid there are typos.
If you don’t like it here, don’t read. I am so tired of people attacking Dr. Glass. There are literally millions of other websites to read.
LikeLike
Thanks for hosting this blog Dr. Glass despite the personal pain it’s meant for you personally. It’s been great to discuss what many are probably thinking. I was an anesthesiologist for 20 years but now Im an attorney who represents patients and their families in medical malpractice lawsuits against hospitals and the government. I was a fervent fan of Joan Rivers and although I didn’t know her personally or care for her as you did, I identified with her, and admired her on many levels. The last time we saw her here in Vegas I laughed until I cried and my belly hurt the next day from laughing so hard. She was a genius and despite what some have said, a wonderful human being who saw the sacredness and worth of every person. She was well ahead of her time and clever in recognizing bigotry and hate by making fun of it. I don’t usually make comments on blogs but I find her sudden unexpected death after a minor diagnostic procedure deeply disturbing and my gut tells me something went very wrong. What happened in this case is unknown and whether there’s blame to cast is not yet known; the dust will have to settle and the facts will have to be exposed. The question you posed at the beginning of this topic is highly appropriate and it needs to be answered. Danial Laird
LikeLike
Please don’t let the idiots scare you away. Your insight and commentary is helpful.
LikeLike
I too share Dr Glass’s deep concerns over why Joan Rivers was deprived of oxygen long enough to cause irreversible brain damage inconsistent w life. I am a Certified Registered Nurse Anesthetist (CRNA). As a CRNA, I manage airways and physiology of patients undergoing all types of surgical procedures, including Endoscopic procedures. We, as anesthesia providers manage patient’s respiratory and cardiovascular responses to the drugs we use to anesthetize them as all patients respond differently. The drugs we use need to have qualified practitioners in airway and cardiovascular management to prevent disasters from happening to patients.
My point being, I read that it was the paramedics who intubated the trachea of Ms Rivers, not any staff at the Endoscopy center. This leads me to believe there was not qualified anesthesia personnel managing her case, because if there were, Ms Rivers would have been intubated immediately and probably not have suffered from prolonged lack of oxygen.
I am speculating about what actually went on at the endoscopy center as I have not read anywhere whether or not they have Anesthesia services providing care for their patients. Most centers do, because it is unsafe to administer propofol without someone there to manage the airway and cardiovascular effects on the patient.
Therefore in light of what happened to Ms Rivers, it leads me to question whether or not her endoscopist had an anesthesia provider with him during her procedure.
Thank you and I send my condolences to Melissa on her mom’s passing.
LikeLike
I have just read Dr Laird’s extremely accurate and pertinent questions regarding the endoscopy of Joan Rivers. I would like to second those questions from not only me, as a CRNA, but from every other Anesthesiologist and Anesthetist I know. We all have the same exact questions and grave concerns. Thank you Dr Laird.
LikeLike
I strongly suspect your suspicion no anesthesia-trained person was there is correct. See my post below (with link to a position paper from the jokers doing endoscopy at Yorkville).
LikeLike
TMZ is reporting that the involved facility employees board-certified anesthesiologists which is good to know if true. Little by little, the facts will come out. Only then will it be possible to make a reliable assessment of what went wrong or that nothing went wrong. Danial Laird
http://www.tmz.com/2014/09/06/joan-rivers-yorkville-endoscopy-clinic-anesthesia-health-department/
LikeLike
I would urge everyone to take a look at the following publication and the author list. The principal author (Cohen) and one co-author (Aisenberg) are both principals at (you guessed it!) Yorkville Endoscopy. They are advocating for propofol administration by the GI endoscopist him/herself.
Click to access pubs-propofol-for-endoscopic-sedation.pdf
Was some anesthesiology-trained provider involved? At this point, no matter what TMZ is saying, I would find it doubtful!
LikeLike
Addendum: Miller is also at that center. In short ALL physician authors on this position paper practice at Yorkville Endoscopy. Sounds like a position of Yorkville Endo.
LikeLike
TY for the link. TMZ readers are being led to believe that everything was in order at the clinic without even knowing what ACLS certification is. They know that their was advanced airway equipment and that all staff had “proper certification”.
Unfortunately the equipment & ACLS certification does not train or certify healthcare workers in the use of advanced airway equipment. Participants in ACLS courses are introduced to the tools that are used. They play with some of the equipment and plastic dummy heads for 40 minutes or so, in a group. The goal is to get an endotracheal tube in through your dummies mouth and check if you did it correctly by inflating the “lungs” (two balloons) through it. Once you have dome that, you move on.
Imagine being shown a violin and bow, being told how they are used, picking up the instrument and learning to play a single note correctly. End of intro to violins and on to the rest of a 2 day course on Classical Music. Pass and you get a Certificate that shows you have been introduced to classical instruments and perhaps some of the great names in music. Are you ready to take over for one of the orchestra’s violinists should they become ill that night? The answer is obvious. In fact, you likely didn’t even notice when his tempo changed or he missed a note.
Dr. Laird, I appreciate your restraint in judgement. It’s unfortunate that you or any anesthesiologist or health care provider who performs intubations would be excluded from a jury (if it comes to that) in the blink of an eye. In fact, either side would likely not want anyone with even a remote connection to healthcare involved in deciding the potential case.
The responses on the TMZ page show that the readers there don’t understand the years of training it takes for anesthesiologists to do what they do. It did no good to have a properly equipped room with no one who knew how to use the equipment.
A final comment re: clinic reporting anesthesiologists employed by them. There’s a lot to investigate there. Are they simply paid to have their name on the list of employees?
LikeLike
Board certification has never been shown to mean anything, as this sad case clearly demonstrates. Indeed, it was the hubris of many “board certified” physicians that allowed this travesty to occur.
LikeLike
Dr. Cohn, I think the article is interesting in light of the questions being asked and I am certainly glad the questions are being raised. However, I have not observed any credible evidence that “Non-Anesthesiologist Administered Propofol Sedation” (NAPS) was used at the involved facility or that an anesthesiologist or anesthetist wasn’t involved in administering sedation or anesthesia to Joan Rivers, whether it was propofol or any other sedatives/hypnotics/analgesics. It is certainly within the standard of care for GI docs to administer non-propofol sedation to endoscopy patients without an anesthetist or anesthesiologist present; it happens every day across the US. Propofol is certainly a trickier drug to use. The facts are slowly coming out; it’s important not to jump to conclusions without all the facts. Really, at this point, very little is known. It really isn’t even clear whether the procedure was a laryngoscopy or upper GI endoscopy and whether a GI doc was involved at all. Any number of things might have gone wrong or it might have been an inexplicable tragedy. NAPS is certainly controversial but it may be only a research interest of some of the docs on staff there. That doesn’t mean it is used at a center at which they happen to be on staff. Nor does it mean NAPS was used on Joan Rivers. It is interesting that both TMZ and Perez Hilton today released statements saying there are board-certified anesthesiologists employed at the facility. Whether an anesthesiologist was involved in Joan Rivers’ procedure is a question that has not yet been specifically answered as far as I know. The facility is in a difficulty place in that i can’t publicly discuss the case while media pundits can openly speculate. This blog has simply asked legitimate questions and I think that’s an appropriate way to handle the issue. More questions should be asked.
Danial Laird
LikeLike
I am counting on you & yours to find out what the hell happened. 99.9% of the time, I’m against a law suit against physicians. Something like this is the exception. The only way to find out is a law suit. If this was an airway death (my strong suspicion), this needs to be not only publicized but broadcast. But come on, Danial… That paper with the coincidence the authors ALL work at that clinic followed by a demise that reeks of an airway death… This is just too coincidental. You’re telling me it walks like a duck, quacks like a duck, but is really a penguin.
LikeLike
I couldn’t agree with you more.
LikeLike
Lol Aaron, I only practice in Nevada; a medmal suit would be handled by New York licensed attorneys, should the family want to pursue such a case and should there be a basis for doing so. I would not be involved.
One thing I’ve learned from practicing law, the facts NEVER turn out to be what you think they are at the start of a case. It’s the attorneys’ job to thoroughly investigate the facts to ensure there are no nasty surprises at trial.
Im not exaggerating when i tell you that at least 99 percent of inquiries about medical malpractice from patients and families turn out not to be cases. There is often no breach in the standard of care, no damages, or the breach isn’t the cause of the damages. Sometimes, you know there is negligence but you know it cant be proven, so there’s no case. Sometimes the patient has so much baggage or is such a difficult personality that you know a jury wont be sympathetic.
The patient or family bringing the suit has the burden of proof. As an attorney representing patients, I look at a medical malpractice case like a producer and director look at putting on a Broadway play. Im ultimately responsible for the financing and every single detail including the cast, the score, the scenery, the lighting, the script, the choreography, etc. Im the one taking the financial risk. The only thing the insurance company defense lawyers have to do to win is to shoot the lead actor in the head. This is usually done by assassinating the victim’s character and finding a way to blame the patient for his or her own injuries- he/she was old, fat, ugly, dishonest, “noncompliant,” going to die anyway, deserved to die, blah, blah, blah. The medical profession thinks medmal lawsuits are a cake walk. They’re actually extremely difficult. Its not a game for the faint of heart. Imagine only getting paid if you win. It’s you and the patient against powerful people in high positions with plenty of money.
This is not to say I don’t understand your point and Im not saying your duck is necessarily a penguin. Im just saying i cant tell what species of bird we’re dealing with because we don’t have access to the facts needed to make the determination. Your inquiries are valid but keep in mind that everyone has a right to his or her good name. Once the facts are known, if there’s legitimate blame, that is the time to place the blame squarely on the responsible individuals. Danial Laird
LikeLike
Yes, I agree. I’ve seen a legal bogosity from the receiving end, forcibly non-suited thanks to the vigorous tort reform we have in Texas. Hence my sympathies in 99.9% of cases are with the physicians. But my god, man… “we don’t know how long joan was hypoxic….” WTF?????!!!!!
LikeLike
Aaron, who said “we don’t know how long Joan was hypoxic”? Was that reported? Thanks, Danial
LikeLike
Danial,
That statement has been all over the reporting from the time Joan arrived at Sinai. Yorkville Endo said it. And I react strongly to the statement because it means either she was down a really long time, and they don’t want to say how long or that she wasn’t monitored. Actually, I think the former possibility (a lie) reflects more favorably on them. It’s the sort of thing that makes me go “WTF?!” and think no anesthesia provider (either BC MD or CRNA) was involved here. We have monitoring standards, you see.
LikeLike
I spoke to a GI doctor associated with the Yorkville Center who told me that the procedure did not have an anesthesiologist present. Anesthesiologists are employed by the center, but one was not readily available when the problem occurred and that none was in the room in association with the procedure. It will be interesting to learn if an anesthesiologist working at the facility will be willing to put his or her neck on the chopping block when they were not there for the procedure and its complications.
LikeLike
STP, can you say with whom you spoke? Did your source say that Non-Anesthesiologist Administered Propofol Sedation (NAPS) was used on Joan Rivers? Danial Laird
LikeLike
Dr. Cohen personally directs the administration of propofol to his patients. I cannot tell you if the person administering the propofol was a nurse or a medical technician. I suspect from what I have been told that the person giving the medications is generally a medical technician directed by Dr. Cohen. I can also tell you that In New York State medical technicians are not allowed to administer drugs to patients even at the direction of a physician. Unfortunately much of medicine in New York and elsewhere is performed by physicians who use seat-of-the-pants logic to make professional decisions based upon their misconception that they are in charge. This includes physicians telling other physicians what to do when patients are referred probably related in part to their application and understanding of the “gatekeeper” concept.
LikeLike
Dr. Glass,
I read your blog all the time, I rarely comment, I am always just so busy.
Out of respect for Joan, I think for this post you should axe the trolls. Just my opinion. I, too, am tired of the attacks on you, everyone has critics and haters, but my goodness, we are talking about a senseless death – not TOT mom. This was NOT a surgery, this was more of an exam, if you will.
. You have repeated your credentials more times than necessary, while we appreciate you not letting trolls hide – I think for Joan and M.D’ s are commenting trying to make sense of this and this was YOUR friend, they are not worth it.
Just spam their asses. Again, just my opinion. That’s not to say I don’t find myself smirking when you call out the trolls either. 🙂
I find myself tearing up when coverage is shown of Joan Rivers. When they said there was a red carpet – what Joan wanted, my husband gave a face; like a shocked one, I told him; at least Joan admitted she wanted it.
I am hearing Yorkville Endoscopy received death threats.
You are appreciated Dr. Glass
LikeLike
Thank you so much for your beautiful words. I have spammed a few of the trolls but wanted to leave some of them up there as an example that if they troll and produce hate they will be be fully exposed. You are right there are too many wonderful comments to help make sense of what the medical people are saying and they should be removed. Thank you.
LikeLike
Here’s some interesting questions being asked by Geraldo Rivera:
http://latino.foxnews.com/latino/opinion/2014/09/09/geraldo-rivera-whowhat-killed-my-friend-joan-rivers/
LikeLike
Now we’re getting somewhere:
http://www.nytimes.com/2014/09/10/nyregion/at-east-side-surgery-center-a-rush-to-save-joan-rivers.html?_r=0
LikeLike
Is this article implying that Joan Rivers’ surgeons decided to do an impromptu vocal cord biopsy in an outpatient surgery center without first securing the airway??
http://www.nydailynews.com/entertainment/gossip/joan-rivers-surprise-biopsy-cut-air-supply-source-article-1.1934178
LikeLike
All I can say is “dumb. f-ing dumb.” if that’s what they did. Unless you can somehow make the case this comes under “other procedures as indicated” it would constitute battery as well.
LikeLike
I posted that too. Didn’t see Dr. Laird posted the link Dr. Glass, my fault.
LikeLike
Did you see the NY DAILY NEWS Dr. Glass??
I am only posting EXTRACTS;
Rivers’ doctor — who identified himself as an ear, nose and throat specialist — asked if he could use their instruments when the clinic’s doctor noticed “something” on Rivers’ vocal chords, according to the source.
“He asked and they let him,” the source said. “ A huge no-no .”
The source added that the “Fashion Police” star had only signed off on an endoscopy — not the far more dangerous biopsy of her vocal chords.
also says;
Last week, a rep for the clinic described the medical facility to ABC News “as a federally and state licensed facility, has the same level of life-saving and resuscitation devices (such as state-of-the-art cardiac defibrillators, airway management equipment, etc.) found in any hospital emergency room or hospital-based operating room.”
Read more: http://www.nydailynews.com/entertainment/gossip/joan-rivers-surprise-biopsy-cut-air-supply-source-article-1.1934178#ixzz3CvJfi9Jj
That 911 call bothered me. There was no sense of urgency, it was like, “um, we have someone who isn’t breathing”
LikeLike
This makes me angry.
LikeLike
Which means that the only one question that was clever was whether there was malpractice or not. The rest is just garbage.
LikeLike
Doug you missed the whole point of the blog It asked the question as to whether there was malpractice and there was indeed. Stop projecting your garbage on to this site. When someone goes in for a simple evaluative procedure and comes out Dead all questions need to be asked . This blog was written as soon as she was rushed to Mt Sinai hospital and these are the things which rushed through my mind Doug. If you had or ever have a loved one in a similar position to what Joan encountered I hope you would ask as many questions as I did and not consider it garbage.
LikeLike
Assuming for a moment these latest leaked “facts” are true, (and that’s a very big assumption) even more questions need to be asked:
1. Did Joan Rivers provide informed consent for the vocal cord biopsy which was allegedly attempted?
2. Did the ENT surgeon who allegedly attempted to perform a vocal cord biopsy have staff privileges at the facility and did he have clinical privileges at the facility to perform a vocal cord biopsy?
3. Did the license of the endoscopy center provide authority to perform ENT procedures such as vocal cord biopsies?
4. Are ENT procedures routinely performed at the endoscopy center?
5. Did the facility have the appropriate surgical instruments available to perform a vocal cord biopsy or, is it possible that gastrointestinal biopsy equipment was jury-rigged to perform this ENT procedure?
6. The vast majority of anesthesiologists are extremely adept at treating laryngospasm in a timely fashion before the onset of severe hypoxemia causing cardiac arrest. If an anesthesiologist was physically present in the procedure room and providing sedation or anesthesia, was the laryngospasm broken immediately by the anesthesiologist?
7. Did the facility have the appropriate medications available to immediately treat refractory laryngospasm?
8. Did the involved health care providers attempt a vocal cord biopsy without first securing the airway with an endotracheal tube? If so, is that within the standard of care?
9. Did the attending physician attempt to stop the outside surgeon from allegedly attempting to perform the vocal cord biopsy? If not, why?
10. Did the facility nurses attempt to stop the outside surgeon from allegedly performing the vocal cord biopsy? If not, why?
11. Did the facility provide its equipment, supplies, procedure room, and personnel to the outside surgeon who allegedly attempted to perform a vocal cord biopsy?
12. Was propofol sedation administered to Joan Rivers during her procedure?
13. Is a vocal cord biopsy usually performed under full general anesthesia?
14. Did the involved physicians allegedly attempt to perform a vocal cord biopsy on Joan Rivers while under propofol sedation?
15. While various reports have stated that the involved facility “employs anesthesiologists,” that really isn’t the issue. The facility website mentions that for certain “complex or lengthy” procedures, an anesthesiologist may be present to administer sedation (Patient Education ERCP). How about for endoscopy with alleged impromptu vocal cord biopsy? The important question is whether there was an anesthesiologist physically present in the procedure room during Joan Rivers’ procedures and immediately available to deal with complications such as laryngospasm?
16. Was “Non-Anesthesiologist Propofol Sedation” (“NAPS”) utilized on Joan Rivers? If so, did she give her consent for the same?
Given that the New York Daily News can’t even spell “vocal cords” correctly, the article lacks a certain credibility. I’m still not convinced there is credible evidence that the facility or the involved personnel committed malpractice. All we have is an unnamed anonymous source who is likely basing his “facts” on second, third, or fourth-hand information. Nevertheless, even if there is only a grain of truth to the article, it raises many more important questions, the answers to which need to be determined.
Danial Laird
LikeLike
EXCELLENT QUESTIONS!!
LikeLike
There is a subtle manipulative undercurrent to the new York Daily News article which I don’t like.
A common defense in medical malpractice cases is to assassinate the character of the patient and blame him or her for whatever goes wrong.
Here, the article alleges a member of Joan Rivers’ “entourage” (this is the first I’ve heard that an “entourage” accompanied her to the procedure) injected himself into the endoscopy procedure and insisted on doing a vocal cord biopsy after another physician noticed something on her vocal cords.
Here’s the unspoken implication: It was really Ms. Rivers’ own people who screwed everything up. Were it not for this pushy member of the Rivers’ “entourage,” everything would have been just fine. In a a way, you see, it’s actually Joan Rivers’ own fault she died. If she hadn’t brought her own pushy doctor along, all would have been well. (Obviously this is complete nonsense since Ms. Rivers was unconscious at the time of the alleged malpractice and is in no way responsible for anything.)
The article has a slippery, self-serving public relations feel that makes my skin crawl. I’m still waiting for the dust to settle. Let’s see what the facts are and let the chips fall where they may.
LikeLike
According to the facility’s statement, much of what appeared in the article referencing a vocal cord biopsy is not true:
http://www.cnn.com/2014/09/10/showbiz/joan-rivers-clinic-responds/index.html?iref=allsearch
LikeLike
Dead weight off a sinking ship?
Whether or not an unauthorized vocal cord biopsy caused this disaster, this is highly suspicious…
http://www.nydailynews.com/new-york/clinic-head-steps-joan-rivers-death-report-article-1.1937694
LikeLike
The question I’d like to know the answer to is this: If somehow laryngospasm was triggered near the end of the procedure, were rapidly-acting paralytic laryngospasm-busting medications (i.e. succinylcholine) immediately available? If so, was succhinylcholine administered? Even refractory laryngospasm can almost always be broken immediately with succinylcholine; the vocal cords cannot adduct if the muscles controlling their movement are paralyzed. If there was no succhinylcholine available, that brings up another long list of concerning questions. Succinylcholine is a very old and inexpensive medication. As far as I know, Joan Rivers had no contraindication to its use. I don’t even want to consider the possibility that Joan Rivers died for want of a $30 bottle of succinylcholine. I continue to wish that when the dust settles, we find out that all that should have been done, was done, and it was just one of those things we can’t explain. At this point, there is so much conflicting information and no doubt, much misinformation. It’s just impossible to tell what actually happened and whether the clinic or any person present that day performed below the standard of care. The more information that’s leaked by the involved medical personnel, the more confusing the story gets. Danial Laird
LikeLike
No Suc on hand at the clinic the NY Times reported yesterday.
LikeLike
From NY Times: One possibility is that she suffered from laryngospasm, a closing of the vocal cords that shuts off the airway. This is often managed with a drug called succinylcholine; that drug was not on hand, according to a clinic spokeswoman.
LikeLike
No sux on hand at the clinic if true is already culpable negligence in my professional opinion. I’ve already stated my belief it’s as important in an anesthetizing location as atropine and epi. Going anywhere near her vocal cords with a scope or anything else without immediate access is criminal. Where do I sign up to testify?
LikeLike
Read this online (Crazy):
They do not have the drug in the possession because having it also requires that you possess the drugs required to treat Malignant Hyperthermia and the machinery to diagnose the disorder as well. Endoscopy centers do not carry these drugs because of the expense of the ones to treat and diagnose Malignant Hyperthermia.
LikeLike
According to the Malignant Hyperthermia Association, the cost of having dantrolene (the treatment for the very rare reaction to succinylcholine) on hand is $3000 per 3 years. I think that works out to around $2.74 per day. Succinylcholine itself is less than $30 a bottle I’d guess.
LikeLike
That’s extremely foolish. The risk of MH is about 1 in 30,000 for a child and 1 in 50,000 for an adult. The risk of mortality in an MH episode is roughly 10% in this age. If Joan had developed full-blown MH and were immediately transferred for emergency therapy, her odds would have been much better than being transferred as she was with a severe anoxic encephalopathy.
I suspect the true reason they don’t keep the sux on hand is that it requires special treatment (needs to be refrigerated) and will go bad over time and need to be reordered. To the clinic, it just seems like added expense, which I guess it is 99.99% of the time. But when you need it, you NEED it. Yes, you can try other things like chin-lift/jaw-thrust, CPAP, IV Xylocaine and additional propofol. But I can tell you if it were severe laryngospasm, those measures would work slowly or not at all, whereas a tiny dose of sux (10 mg in an adult)…. 10% of an intubating dose, will break it almost immediately.
LikeLike
Who can administer what drugs in what setting is usually a matter of state law and regulation. However, it is not uncommon for flight paramedics and rural hospital emergency rooms in the western US to use succinylcholine for airway emergencies and not have dantrolene on site in the unlikely event of an episode of MH. It’s simply a matter of risk benefit analysis.
Additionally, it s a MINOR inconvenience to stock dantrolene. It almost always expires without being used (thank goodness) but the cost of having the maximum adult dose on hand is less than $3 per day. Having a stock of dantrolene is really a de minimis expense in a busy facility with an operating budget in the millions of dollars. The risk of having an airway emergency in an endoscopy clinic, particularly one where propofol is used, is far greater. The risk of Joan Rivers having malignant hyperthermia is almost zero, given her age and number of previous procedures.
What really happened and whether any person is culpable, or whether the facility is culpable, is of course not yet known and there is serious question about the veracity of “facts” already leaked by the medical personnel involved.
I’m very curious to learn the identity of the ENT surgeon and whether more than a laryngoscopy,was done. I can’t imagine that the nurses at the facility did not ask the identity of every person entering the procedure room, particularly if the outside physician was permitted to perform a procedure on a patient rendered unconscious and vulnerable in their facility. Some reports said the ENT was female. She’s also could be a sub specialist in laryngology. That has to be a rather small group of people, even on Manhattan.
LikeLike
MH is vanishingly rare even taking all comers. It’s lethality if it does happen is far less than 100%, and the harm to the patient in waiting 10 minutes to treat during a harried trip to Mt. Sinai is far less than the lethality of a complete airway obstruction, which will have a 100% lethality within 10 minutes.
The most galling thing about this is, IF (BIG IF) they were even doing a laryngoscopy without a biopsy, there was absolutely no doubt about what was happening as they could watch it occurring, but were unable to effectively treat. Even during a GI endoscopy, you can see the vocal cords, and therefore should have a very good idea laryngospasm is occurring.
LikeLike
I believe it’s a case of the wrong specialists doing the wrong procedure in the wrong place. When something went wrong they were in over their heads. Perfect storm for disaster. I wish she had gone to the renown doctor Steven Zeitels at Mass General. From what I have read he has pioneered several vocal cords surgeries and is an expert in micro surgery. It seems dubious that Joan Rivers had acid reflux. She was so prolific and passionate that I imagine she talked non stop all day long. I bet Zeitels could have repaired the damage safely.
LikeLike
Have you heard the latest Dr. G? About the make up artist? This is getting crazier by the day.
I saw the exclusive that you have Radar on Line. I am glad you said what did – Joan did not have to die.
People seem to forget, what Joan was supposed to have done was NOT surgery and keep bringing up the age factor, it drives me NUTS. Back to what Joan was supposed to have done and what was done is obviously what did not happen.
LikeLike
I had laryngitis five years ago – you know what my Dr. told me to do? Not to talk for a week. LOL. I swear, it helped.
LikeLike
That’s right Dr. G.!
LikeLike
Since so much has surfaced now since I first wrote this blog questioning whether there was malpractice I have some additional thoughts I would like to share with you.
Now that we know a gastroenterologist was involved, he was most likely checking for esophageal reflux as that would have been proper considering his expertise.
To provide VIP treatment in both saving Joan time and giving her a diagnosis more quickly,he called in an ENT consult to give her opinion, in case he didn’t find esophageal reflux during his exam.
That is why he introduced the ENT to his staff as an observer. He didn’t call her a colleague or an associate but rather ” an observer” which I think is very significant as it seems that his initial intention was to merely have her observe.
But maybe the ENT had other ideas in mind as she brought with her a large bag which the staff thought contained makeup. Hence it is understandable that the staff thought this “observer” was there to put on Joan’s makeup after she finished her medical procedure so that when she exited the clinic she would look camera ready for any paparazzi.( I refer to the ENT as a she becuause TMZ mentioned it was a she when they discussed the this makeup artist perception by the clinic’s staff.)
But the ENT did not just observe.Instead, she decided to take action with the approval of the head of the clinic. He even lent her his instruments to perform the biopsy. In essence, even if he initially thought of the ENT as an observer,he allowed someone who wasn’t authorized to do surgery rather than merely observing.
Both the gastroenterologist and the ENT may have figured, since Joan’s vocal cords were already visible now that she was under, the ENT could just take a little snip of the tissue and put it in a vial that no doubt she carried in her black back which she brought with her. She obviously thought she could cut corners and not follow the proper protocol.
What she needed to have done was ONLY observe. Then she needed to schedule Joan for a proper surgery in a hospital where Joan could be intubated properly and monitored by an anesthesiologist, biopsied and removed the alleged mass on her vocal cords via laser or surgery.
When the ENT cut corners so to speak, she didn’t plan on the vocal cords going into laryngospasm and Joan’s airway being cut off and her dying. The clinic was most likely unequipped to handle laryngospasm and quickly the remedy the situation of succinylcholine since they usually work on the opposite end of the alimentary canal.
The gastroenterologist should NOT have allowed the ENT do so the biopsy or to touch the patient for that matter. He only needed to allow her to OBSERVE.
It is questionable that Joan signed off ont he ENT’s biopsy when it may not have been planned in the first place. The ENT seems like she is in huge trouble for this.
To me it seems like a clear malpractice case. With the clinic, gastroenterologist, and ent being liable, I have no doubt that their respective malpractice carriers will pay top dollar for this tragedy. But these doctors may still have worries. If they are sued for an amount not covered by their policies, they may be personally liable for the rest of the money which may possibly bankrupt them. But what about criminal charges against them? Could the gastroenterologist be charged as an accessory to second degree manslaughter? Will the ENT be charged with secondary manslaughter and or battery? Will she have the same fate as Dr. Conrad Murray and do prison time for a number of years?
LikeLike
Medical executive committees at freestanding ambulatory centers, are seeing incidents where a surgeon thinks because he/she is operating at an asc, it’s the “wild wild west” and they can pretty much do as they please. It’s very unpleasant for all concerned to disabuse them of that fact. As the medical director of that endo center, Cohen was certainly on such a committee and should have known the consequences for putting the facility at risk like this. I am more forgiving of him with respect to not understanding the possible outcome of this course, as he’s not an airway expert.
As a BC anesthesiologist whose area of academic and clinical expertise (when in academia) was difficult airway management, the picture of a patient anesthetized under propofol, positioned on her side and undergoing a vocal cord biopsy without a contolled, protected airway should have set off loud alarm bells for anybody with training similar to mine. But putting myself in this situation, it’s difficult. Beyond registering a verbal objection, and perhaps offering forcefully to tracheally intubate the patient before proceeding, what could he/she do? Physically grab the instruments from the hand of the surgeon? Set up a body block between the ENT and the patient, while managing an anesthetic? The anesthesiologist (if there was one) was trapped and can’t simply withdraw from the case; the medical board would consider that patient abandonment. But I also couldn’t fathom any well-trained anesthesiologist working at a center without succinylcholine. Last week, I had a patient laryngospasm during a colonoscopy with her saturation dropping. Sux 10mg (half cc) and it was all fixed. Educated the endoscopist even “hear the patient singing to you? that’s laryngospasm.” For an ENT, driving this, it’s an act of unfathomable stupidity. Does it approach the level of a Conrad Murray criminally negligent homicide? That’s for a jury.
One thing I can tell you. Whatever malpractice coverage that ENT has won’t cover this incident in a facility where she had no privileges.
The facility is denying a biopsy took place. But I think a lawyerly parsing of their statement is in order. Did they say, “this facility does not do biopsies of vocal cords.”? Well, if the procedure was performed by somebody not credentialed at the facility, maybe the statement is still true. Or maybe they attempted the biopsy but she went into tight laryngospasm before it could be accomplished. What I’m saying is this story is just too strange and has too many odd details to be a complete fabrication.
LikeLike
I enjoy your well-informed comments Dr. Glass. I think Joan Rivers got one of her wishes in that her death is anything but “boring.” Her quote below about dying of “natural causes” makes me laugh and cry in the same paragraph. Her death will be discussed for years and the mass media attention aside, her death has provoked serious discussion about several medical controversies. Her eleven o’clock number was really quite something, she died interesting! I only wish the circumstances were not so heartbreaking. Danial Laird
“I hate people who die of natural causes; they just don’t understand the moment. It’s the grand finale, act three, the eleven o’clock number — make it count. If you’re going to die, die interesting! Is there anything worse than a boring death? I think not. When my time comes I’m going to go out in highs type. I have no intention of being sick or lingering or dragging on and on and boring everyone I know. I have no intention of coughing and wheezing for months on end. One morning you’ll wake up and read a headline: Joan Rivers Found Dead…On George Clooney’s Face. Clooney Was So Bereft All He Could Say Was, ‘Xjfhfyrnem.'”
LikeLike
I am shocked that we have just discovered that the ENT who was unauthorized to do the biopsy in the first place had the audacity to take a selfie with Joan while Joan was under anesthesia. This is unconscionable. This ENT physicians should lose her license for such unprofessional behavior. Apparently Melissa is going to sue her along with the endoscopy clinic and the gastroenterologist.
h
http://www.cnn.com/2014/09/16/showbiz/joan-rivers-clinic/“>
LikeLike
Good Lord, if this is true, it demonstrates extremely poor judgment on the part of the surgeon and everyone one who allowed it to happen. Wanting to be photographed with an unconscious unresponsive patient is a very special kind of creepy. I would love to hear what a psychologist had to say about it.
Having anesthetized approximately 20,000 patients, I’ve never once encountered a surgeon, nurse, or staff member who wanted to photograph themselves with an anesthetized patient.
If the surgeon did actually take a selfie, WHY? If the surgeon wanted a photograph with Ms. Rivers, why not ask before or after Ms. Rivers was anesthetized? If true, this kind of thing is a violation of Ms. Rivers’ privacy and is just damn weird.
Most operating room nurses I know would never allow such ridiculous offensive behavior in an operating room or a procedure room. Doesn’t the registered nurse act as the patient’s advocate and the patient safety officer in the operating room??
LikeLike
It didn’t say JR was in the selfie, but I agree if that was done, it is a sign of emotional illness. The whole thing, as described, sounds like malignant narcissism to me (though I’m not a psychiatrist and don’t even play one on tv).
Horrible judgement beginning to end by all the doctors involved in this.
LikeLike
http://www.cnn.com/2014/09/16/showbiz/joan-rivers-clinic/
LikeLike
Now we know there will be a malpratice suit by Meliisa against the clinic, the gastroenterologist, and the ENT doctor. We know the the ENT was Dr. Gwen Korovin. How sad for everyone involved. Her career is essentially over and Joan is dead.http://www.tmz.com/2014/09/17/joan-rivers-doctor-death-throat-surgery-gwen-korovin/
LikeLike
I feel sorry for her. Who wants to go through life as the doctor who killed Melissa Rivers. Maybe she just had a “thinko”. Unfortunately a thinko like this can kill IF (big IF) it’s as described. Really big thinko.
LikeLike
I mean Joan Rivers. I guess I had a thinko myself.
LikeLike
If what Dr. Korovin says is true and she didn;t take a selfie and instead took a photo of Joan’s vocal core, the source at the Clinic may be sured to liable and CNN is definitely in trouble for reporting wrong information. So Korovin’s potential defamation suit again CNN and her suit against the clinic and staff for saying she did something she may not have done will help pay for her own legal defense. What a mess!
http://www.tmz.com/2014/09/18/joan-rivers-death-selfie-gwen-korovin-doctor-yorkville-endoscopy-clinic/
LikeLike
She may have taken a picture of herself and/or Rivers with the laryngoscope/endoscope as a “test image”. I’ve seen surgeons do that. This would give her plausible deniability for the charge she was making a “selfie”. May have been perfectly innocent… or not!
LikeLike
I’m inclined to believe that she did not take a selfie here. This was not some starstruck doctor, but someone who was used to dealing with famous people. Her office is apparently full of pictures of celebrity patients, and I am sure that Joan would have agreed to pose with her, if she was in fact her personal doctor.
LikeLike
I agree. Now that we know who she is and her star clienetele, she most likely may have taken a photo of the vocal cords and this staff member may have mistaken it for a selfie.If it is the case, the staff member needs to be sued for literally destroying the doctors reputation along with CNN who reported the alleged incident.
LikeLike
Dr. Korovin lost her reputation by performing an unlawful procedure in a facility that was inequipt to handle such a procedure. In addition, she likely does not hold the skill set to perform surgical procedures with her VIP practice. I’m sure she hasn’t done a real procedure in years. Furthermore, her knowledge and judgement are questionable illustrated by her quackery administration of a b12 shot in the rear to Ariana Grande for a cold before her appearance on late night TV. B12 has has proven zero efficacy. At a minimum “Dr.” Korovin should lose her medical license and go to jail for manslaughter.
LikeLike
The New York Times has a well done article about VIP Syndrome. The Times has done a very good job covering this issue. They’re one of the few news sources that hasn’t ended up with egg on their face from reporting “facts” that actually aren’t known to be facts. I strongly agree with the notion that getting health care providers off their game is an invitation for disaster. So-called VIPs need to be treated like everybody else; it’s in the best interest of the patient. There are very good reasons for the way things are usually done.
Danial Laird
http://www.nytimes.com/2014/09/22/nyregion/joan-rivers-treatment-seen-as-possible-example-of-vip-syndrome.html?_r=0
LikeLiked by 1 person
I agree completely. Where I live in Beverly Hills, you see this all the time.There is VIP treatment by doctors who are so star struck they would do anything above the call of duty for the patient even if it meant bending the rules, which they often do.
That is most likely what happened here.It seems that corners were cut and steps were left out to the detriment of the patient. Sometimes being a celebrity does not get you the best treatment.
In my practice where I had a great number of celebrity patients I treated them as I would treat anyone who did not have celebrity status- with the same respect as evryone was treated with equal status. Unfortunately this is not the case with many.
LikeLike
Dr. Glass, Was wondering if you could do an update on Joan?
LikeLike
Dr. Glass,
Was wondering if yo could do an update?
LikeLike